Although total hip replacements generally yield excellent outcomes, revision surgery may still be necessary for various reasons. Fortunately, such revisions are now far less common than in the early days of hip replacement surgery. The most frequent causes for revision are implant wear and infection.

While pre-operative planning is important for all joint replacement surgeries, it is absolutely critical in revision hip surgery. Thorough planning ensures that multiple surgical options are available, allowing the surgeon to respond effectively to intraoperative findings
BLOOD LOSSRevision hip surgery typically involves a more extensive surgical approach and complex bone reconstruction, often resulting in greater blood loss compared to primary total hip replacement. To reduce the need for blood transfusions, a Cell Saver system is employed during the procedure. This technology allows for the collection, filtration, and reinfusion of the patient's own blood lost during surgery, thereby minimizing transfusion requirements.
 The most common cause of failure nowadays is loosening of the one (commonly the socket component) or both components.
The most common cause of failure nowadays is loosening of the one (commonly the socket component) or both components. Infected hip replacement that usually requires either one-stage or two-stage revision.
Infected hip replacement that usually requires either one-stage or two-stage revision. Sometimes it is necessary to revise the hip because it is unstable and dislocates or slips out of the joint frequently.
Sometimes it is necessary to revise the hip because it is unstable and dislocates or slips out of the joint frequently. Relatively rarely, surgery may be required because of bone loss caused by particles generated from wearing down of the replacement. This condition is called osteolysis.
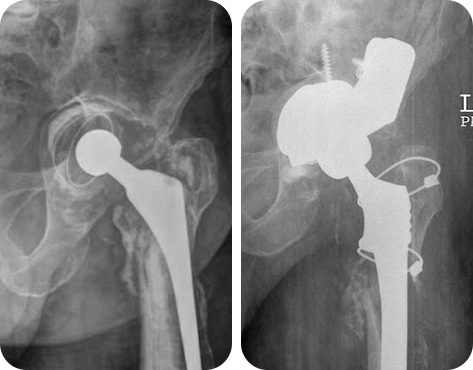
Relatively rarely, surgery may be required because of bone loss caused by particles generated from wearing down of the replacement. This condition is called osteolysis. Fracture around the implants, particularly on the femoral side usually requires revision of the implant.
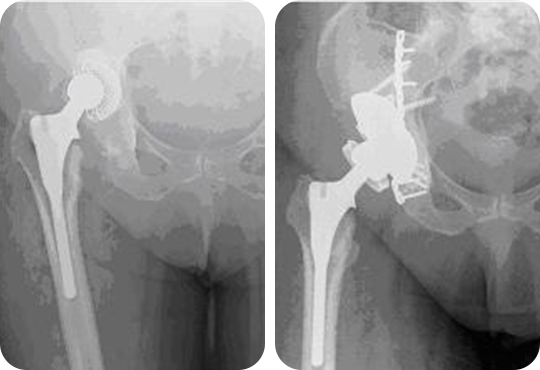
Fracture around the implants, particularly on the femoral side usually requires revision of the implant.The implants used in revision hip surgery are broadly similar to those used in primary procedures. However, in many cases, the components required for revision are more complex and must be carefully selected based on the individual patient's clinical situation. The socket (acetabular) component used in revision surgery is typically uncemented, relying on press-fit fixation that is often reinforced with screws to secure the cup to the pelvic bone. In cases where there is significant bone loss around the failed original socket, standard implants may not provide a stable fit. These defects can be managed using bone grafts or specialized components with modular extensions designed to better fill and support the deficient areas. In rare and severe cases of bone loss, additional support may be required in the form of reconstruction cages or fixation plates, which act as scaffolding to provide structural stability and facilitate implant fixation.

Regarding the femoral component, it is crucial to remove the failed implant carefully to avoid further bone loss. In some cases, this may require a controlled longitudinal split of the upper femur (extended trochanteric osteotomy) to facilitate safe removal of the old implant. The new femoral implant is typically inserted using an uncemented technique. These implants often come with modular 'add-on' options, allowing the surgeon to customize the construct intraoperatively for optimal fit and stability. This modularity provides a wide range of component combinations, enabling tailored reconstruction based on the patient’s specific anatomy and bone condition. In certain situations, a strut bone graft may be used to reinforce structural integrity and encourage new bone growth in areas with significant bone loss.
The outcome of a revision hip surgery depends on various factors including the cause for the revision procedure. Prof Kavarthapu will provide you with specific information on the expectation following your revision hip replacement procedure.
