Femoro-Acetabular Impingement syndrome (Hip Impingement) is caused by unwanted contact between the head of the thigh bone and the hip socket, resulting in damage to the Labrum and the joint lining cartilage and decreased range of hip movement. It is usually due to excessive bony growth at the front of the femoral neck ('bump') that impinges on the front edge of the socket damaging the labrum and joint cartilage during normal range of motion. This can also be due to the presence of a deep socket or facing of the socket in the wrong direction. The patient typically experiences sharp hip pain during deep hip flexion and rotation movements. Although scientific evidence is still slightly sketchy, it is felt by many that patients with hip impingement, if untreated, carry an increased risk of developing osteoarthritis ('wear and tear'), with the subsequent requirement for either a hip replacement or other major hip operations. Hip arthroscopy can be used to reshape the femoral head and socket to prevent impingement, and can potentially protect the hip joint from developing / slowing down osteoarthritis, as well relieving current symptoms.
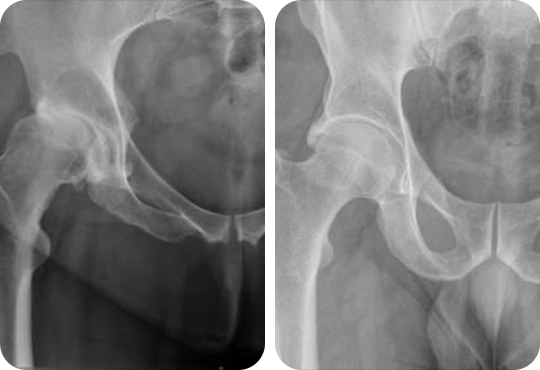

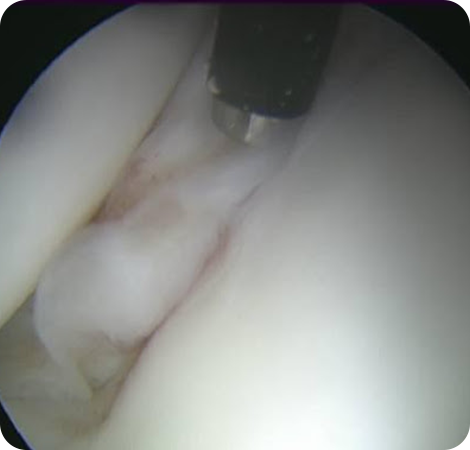
The labrum is a ring of cartilage that is present around the rim of the socket surrounding the acetabulum. This can be found to be partially damaged or torn in some patients. This is usually associated with hip impingement. During hip arthroscopy labral tear can be either debrided (remove the damaged tissue only) or repaired. MRI and/or CT scans, although often performed before hip arthroscopic surgery is undertaken, do not always reveal every labral tear.
The treatment may initially consist of a trial of non-operative measures such as activity modification, pain medication and physiotherapy. If appropriate, hip arthroscopy may be considered.
Hip Arthroscopy
 The surgery is generally performed under general anaesthetic.
The surgery is generally performed under general anaesthetic. The bones of the hip joint (the ball and socket) are separated by approximately 1cm by applying traction to the leg with a special device. This provides enough space in the hip joint to allow insertion of a small telescope camera (arthroscope) into the joint safely. Further two or three small incisions are made to insert special instruments that allow carrying out of the surgical procedure. The procedure is carried out under the guidance of x-ray control.
The bones of the hip joint (the ball and socket) are separated by approximately 1cm by applying traction to the leg with a special device. This provides enough space in the hip joint to allow insertion of a small telescope camera (arthroscope) into the joint safely. Further two or three small incisions are made to insert special instruments that allow carrying out of the surgical procedure. The procedure is carried out under the guidance of x-ray control. The duration surgery will vary depending on the type of pathology in the hip joint but can last from 45 minutes to 120 minutes, or even more. The hip distraction is used only during part of this procedure.
The duration surgery will vary depending on the type of pathology in the hip joint but can last from 45 minutes to 120 minutes, or even more. The hip distraction is used only during part of this procedure. At the end of the procedure a local injection is given around the incisions to minimise pain after the surgery. The incisions are closed with stitches and covered with sterile padded dressing.
At the end of the procedure a local injection is given around the incisions to minimise pain after the surgery. The incisions are closed with stitches and covered with sterile padded dressing.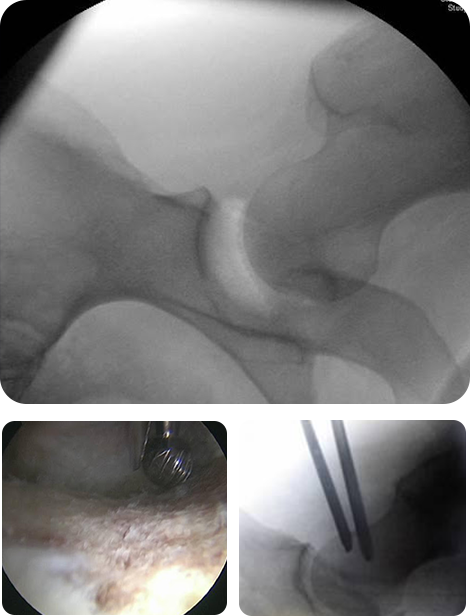
 Usually, you will feel some discomfort in your operated hip area and in addition, mild discomfort can be experienced in the lower back, buttock, knee and ankle regions. The discomfort can normally be reduced with the appropriate routine pain relief. In the majority, there will be some swelling in the groin, buttock and thigh. This is caused by the fluid used during the surgery. The swelling reduces within a few days.
Usually, you will feel some discomfort in your operated hip area and in addition, mild discomfort can be experienced in the lower back, buttock, knee and ankle regions. The discomfort can normally be reduced with the appropriate routine pain relief. In the majority, there will be some swelling in the groin, buttock and thigh. This is caused by the fluid used during the surgery. The swelling reduces within a few days. You will be seen by a physiotherapist on the ward following surgery and will be given instructions regarding mobilising partial weight bearing using crutches. The duration of crutch weight bearing is usually for 2 weeks. However this can be variable depending on what is done during surgery and Mr Kavarthapu will explain to you after surgery regarding this.
You will be seen by a physiotherapist on the ward following surgery and will be given instructions regarding mobilising partial weight bearing using crutches. The duration of crutch weight bearing is usually for 2 weeks. However this can be variable depending on what is done during surgery and Mr Kavarthapu will explain to you after surgery regarding this. Once the physiotherapist is happy with your progress, you will be discharged home the next day with a gentle exercise regime. However the duration of stay can be variable depending on what was done during surgery. You will usually be given a copy of the pictures taken during surgery and we request you bring these copies to Mr Kavarthapu's s clinic during review in 2 weeks.
Once the physiotherapist is happy with your progress, you will be discharged home the next day with a gentle exercise regime. However the duration of stay can be variable depending on what was done during surgery. You will usually be given a copy of the pictures taken during surgery and we request you bring these copies to Mr Kavarthapu's s clinic during review in 2 weeks. The ward nurse would give instructions to remove the outer padded dressing after 2 days, but leave the inner sticky dressings on the surgical wounds untouched. You are given instructions to observe the wound for any signs of infection (increasing pain, redness or swelling).
The ward nurse would give instructions to remove the outer padded dressing after 2 days, but leave the inner sticky dressings on the surgical wounds untouched. You are given instructions to observe the wound for any signs of infection (increasing pain, redness or swelling). You should limit your activities to routine short distance walking using crutches. Please carry out the routine home exercises recommended by the physiotherapist.
You should limit your activities to routine short distance walking using crutches. Please carry out the routine home exercises recommended by the physiotherapist. You will usually receive a call from Mr Kavarthapu's secretary after about 2 days enquiring about your progress.
You will usually receive a call from Mr Kavarthapu's secretary after about 2 days enquiring about your progress. Following your discharge, you will usually be reviewed in the clinic for 2 weeks. At this appointment, your wound may be inspected and the sutures removed. A further explanation of the surgery undertaken can then be provided using the operative pictures. You will usually be referred to physiotherapy at this point if the assessment reveals satisfactory progress. Further appointments will be made after 6 weeks.
Following your discharge, you will usually be reviewed in the clinic for 2 weeks. At this appointment, your wound may be inspected and the sutures removed. A further explanation of the surgery undertaken can then be provided using the operative pictures. You will usually be referred to physiotherapy at this point if the assessment reveals satisfactory progress. Further appointments will be made after 6 weeks. Your physiotherapist will develop an appropriate rehabilitation programme according to Mr Kavarthapu's protocol. Your physiotherapist will guide your return to sporting activities (running etc.) depending on your progress. This is extremely variable between individuals, depending on the surgical findings and the length of symptoms prior to surgery.
Your physiotherapist will develop an appropriate rehabilitation programme according to Mr Kavarthapu's protocol. Your physiotherapist will guide your return to sporting activities (running etc.) depending on your progress. This is extremely variable between individuals, depending on the surgical findings and the length of symptoms prior to surgery. In the majority, by 8 weeks after surgery you should be walking relatively pain-free. Medium impact activities such as jogging can usually be commenced by this time, and you can gradually progress to running if there is a satisfactory progress. Remember, however, that it may take 3 to 6 months (or more) to return to an elite level of competition/fitness. Any unexpected increase in pain can be treated with ice pack application and anti-inflammatory medication. The broad strategy for rehabilitation is to regain early range of movement and stability, followed by strength and endurance. Returning to work will depend on pain levels and the nature of your job.
In the majority, by 8 weeks after surgery you should be walking relatively pain-free. Medium impact activities such as jogging can usually be commenced by this time, and you can gradually progress to running if there is a satisfactory progress. Remember, however, that it may take 3 to 6 months (or more) to return to an elite level of competition/fitness. Any unexpected increase in pain can be treated with ice pack application and anti-inflammatory medication. The broad strategy for rehabilitation is to regain early range of movement and stability, followed by strength and endurance. Returning to work will depend on pain levels and the nature of your job. Prolonged standing / walking, especially on hard surfaces.
Prolonged standing / walking, especially on hard surfaces. Heavy lifting
Heavy lifting Squatting / crouching
Squatting / crouching Sleeping on your side. Try to sleep on your back. If you must sleep on your side, sleep on the unoperated side, with a pillow under your operated leg - to hold that leg level with the body.
Sleeping on your side. Try to sleep on your back. If you must sleep on your side, sleep on the unoperated side, with a pillow under your operated leg - to hold that leg level with the body. Clutch use in manual cars for left hips and brake usage for right hips may flare up symptoms during the first month and is best avoided. One should do a trial with 'emergency stop brake' safely before commencing driving.
Clutch use in manual cars for left hips and brake usage for right hips may flare up symptoms during the first month and is best avoided. One should do a trial with 'emergency stop brake' safely before commencing driving. Sitting with the hips at 90 degrees a more open seat angle is recommended i.e 120 degrees. Car seats should be tilted backwards slightly in order to open the hips out.
Sitting with the hips at 90 degrees a more open seat angle is recommended i.e 120 degrees. Car seats should be tilted backwards slightly in order to open the hips out.All surgery carries risks, although every effort is made to minimise them. The complications can be temporary or permanent. Reassuringly, permanent complications following hip arthroscopy are rare and the majority are temporary. There are, however, risks which include the standard risks of undergoing general anaesthesia and specific risks associated with hip arthroscopy. Complications have been reported to occur in up to 5% of patients and are most often related to temporary numbness/altered feeling in the groin and genitalia. This is due to a combination of distraction of the hip joint and pressure on the nerves in the groin at the time of surgery. This is uncommon and although there is a theoretical risk that this numbness could be permanent, in the majority the numbness recovers fully, usually within a few days. Other complications that were reported include, but are not limited to: pressure sores and blistering, infection, fracture, increased pain, impotence, bleeding, nerve palsies, abandoned procedure, deep-vein thrombosis, instrument breakage, avascular necrosis of femoral head, extravasation of irrigation fluid, delayed wound healing, exacerbation of symptoms. However, many of these complications are extremely rare. For example, the exact rate of infection following hip arthroscopy is unknown, but would certainly appear to be substantially less than 1 in 1000 Recently NICE produced guidelines on surgical management of hip impingement.
Prof Kavarthapu scientific article on hip arthroscopy can be accessed here: https://link.springer.com/article/10.4103/ortho.IJOrtho_12_18